|
Impacted Wisdom Teeth - Risks of Keeping Them In
The information presented on this site is of personal opinion and consequently is slanted and biased and not based on proper scientific research. The information presented is NOT written by a dental expert. Further the information presented has NOT been subjected to peer review by experts to verify accuracy and data integrity.
First off, everyone should be brushing their teeth at least two to three times a day and flossing at least once a day. Ask your dentist or dental assistant to show you proper brushing and flossing technique. Visiting the dentist twice a year (every 6 months) for a check up and dental prophylaxis is a typical time period for many. (For example the National Health Service (NHS) Dental Services in a 6 month study period in 2010 found that 71% of patients in the U.K. were having a dental check up every 9 months; however, they also feel the interval between visits may be shorter than necessary and this is a source of unnecessary treatment). [57]
The interval between dental examinations should be determined by the individual needs of the patient and assessment by the dental team. (A healthy adult may be able to go up to 2 years between cleanings. Children and adolescents should not go longer than 1 year between dental check ups). [55, 56] If a wisdom tooth or wisdom teeth is healthy (and all teeth) everyone should be closely practicing prevention in order to help avoid large costs, inconvenience, and pain that could potentially arise in the future.
Those who have a wisdom tooth or wisdom teeth (beyond their late teenage years) should have a dentist or other experienced clinician exam the wisdom tooth or wisdom teeth at least every 2 years and preferably every 12 months to 18 months. 18 months is typically how long it takes for a small cavity to become large and infect the tooth's nerve and for gums to become badly diseased. X-rays should also be regularly performed with the interval between examinations determined by the individual needs of the patient and assessment by the dental team. This is to help avoid developing symptoms, damage, and disease that could potentially occur as discussed further below. [13, 14, 66]
Those who have a wisdom tooth or wisdom teeth should certainly be eating healthy and exercising regularly.
The most probable age for a wisdom tooth to erupt is around 20. [36] It is not well known what percentage of impacted wisdom teeth develop disease or symptoms that require their removal. This is because a large number of individuals have had their wisdom teeth removed in the name of prevention in the past so data showing the onsent of pathology in wisdom teeth is not very reliable. [16]
The following studies show how many patients had at least one wisdom tooth removed after a period of time:
In a study of 228 patients (aged 16 to 30 years) over a 5 year period in the U.K. which monitored their lower impacted wisdom teeth, 71 of these patients (32.4%) had wisdom teeth extracted during the 5 year period (9 of the original 228 patients had incomplete data). 66 of these patients had pericoronitis at the start of the study and 23 (34.8%) had wisdom teeth extracted due to recurrent pericoronitis. 153 of these patients did not have pericoronitis at the start of the study and 48 had wisdom teeth extracted (31.4%). The reasons for the extraction in these 153 patients included pericoronitis in 30 patients (19.6%), cosmetic/orthodontic reasons in 6 patients (3.92%), difficult to clean in 4 patients (2.61%), early carie (cavity) in second molar (tooth next to wisdom tooth) in 4 patients (2.61%), painful when eating in 2 patients (1.31%) and earache/TMJ pain in 2 patients (1.31%). [29]
In a study of study 81 patients (aged 20 to 32 years) over a 12 year period in Finland which monitored their wisdom teeth, 54 of these patients (66.7%) had at least one wisdom teeth extracted during the 12 year period. 33 of these 54 patients (61.1%) had at least one wisdom tooth removed despite not having any symptoms. Hence 21 of the 81 patients in the study (25.9%) had at least one wisdom tooth removed due to symptoms associated with the wisdom tooth. [30, 36]
In one journal article [81] exploring how many patients have asymptomatic disease free wisdom teeth two studies were discussed. The first study consisted of 409 asymptomatic volunteers with a mean age of 25.1 years. 119 (29%) of the patients in the study were also free of disease (according to the definition provided in the article). The second study consisted of 249 patients with a median age of 25 years of which 29 (11.6%) had all asymptomatic and disease free wisdom teeth with a total of 855 wisdom teeth (37.3%) being asymptomatic and disease free.
In [80] 146 patients split into a younger patient group (<25 years old) and an older patient group (>25 years old) had their wisdom teeth monitored for less than a four year follow up and a four year follow up. The mean age of the patients in the four year follow up in the younger group was 19.1 years old and in the older group was 34.3 years old. The younger patients (<25 years) had 50 (33.3%) of 150 wisdom teeth erupt after a four year follow up. Older patients (<25 years) had 17 (19.3%) of 88 wisdom teeth erupt after a four year follow up.
In [33], 43 patients with a mean age of 19.1 at the start of the study, had their wisdom teeth monitored for four years. After the four year follow-up period, 15 of 52 (28.8%) in the maxilla and 16 of 66 (24.2%) in the mandible of wisdom teeth became erupted above the occlusal plane of the adjacent second molar.
Many wisdom teeth are impacted and they later erupt and emerge normally or they may never complety erupt. The following studies show how many patients wisdom teeth that were initially impacted had become fully erupted after a period of time:
In a study of patients (aged 18 to 26 years) involving participants from the Dunedin Multidisciplinary Health and Development Study (DMHDS) over a 8 year period in New Zealand which monitored their wisdom teeth, 821 had at least 1 wisdom tooth at the start of the study and 332 (40.4%) had at least one wisdom tooth extracted during the study period. There were initially a total of 2652 wisdom teeth present amongst all subjects of which 790 (29.8%) were extracted. Of the wisdom teeth that were impacted at age 18, 36.2% (295 out of 814) became fully erupted by age 26. [34]
In a study of 36 patients (mean age 19.7) over a 4 year period involving particpants in Jordan there were initally 67 wisdom teeth present amongst all subjects, of which 46 were unerupted with inclinations of 5 to 30 degrees (impacted). Of these initially impacted wisdom teeth 17 (37%) became fully erupted after the 4 year period. [47]
In a study of 237 patients (median age 25.9) over a minimum two year period involving participants from Kentucky and North Carolina there were initially 948 wisdom teeth present, of which 146 upper (maxilla) and 64 lower (mandible) wisdom teeth were unerupted (below the occlusal plane) and vertically or distally impacted. Of these initially impacted wisdom teeth 41 (28.1%) upper and 18 (28.6%) lower became fully erupted after the at least 2 year follow up period. [53]
Phillips and White in 2012, [78] reviewed longitudinal studies focused on the changes of position in wisdom teeth. They identified 5 studies for inclusion which included [33, 34, 36, 53, 80]. In their discussion they state that estimating the eruption of a third molar for the population is difficult and may be impossible for an individual. They say ideally individuals at risk for changes in the angulation or position of impacted M3s sufficient for exposure to the oral cavity should be identified based on clinical risk markers; however, current data does not allow for such model predictions to exist.
A key takeaway from these studies is that horizontally impacted wisdom teeth angled at 35 degrees or greater appear to be least likely to erupt (particulary mandibular horzontally impacted wisdom teeth). [34, 46, 47, 53] In [34] it was reported that fewer mandibular wisdom teeth erupt then maxillary wisdom teeth. Of the maxillary wisdom teeth not extracted, distoangular were the least likely to erupt. Of the mandibular wisdom teeth not extracted, horizontal and mesioangular were the least likely to erupt. In [36] more maxillary wisdom teeth (14%) than mandibular wisdom teeth (5%) not initially visible in the mouth (18 years prior) had erupted. In [53] mesially/horizontally impacted wisdom teeth were least likely to erupt when compared to verticaly and distally impacted wisdom teeth. Only 3% of mandibular wisdom teeth with an initial angle of 35 degrees or greater erupted. As such mesially/horizontally impacted lower wisdom teeth may lead to caries (cavities) in adjacent (second) teeth (molars) [84].
One study performed actuarial life-table analysis and looked at 583 patients over a 1 year period who had at least one lower impacted wisdom tooth and determined that older patients were inversely associated with the development of symptoms (meaning older patients are less likely to develop symptoms than younger patients). [51]
Several studies have explored the impact of the NICE guidelines in the U.K. They have found that the same number of wisdom teeth before the guidelines were implemented are extracted as after. In addition the age of the patient having extraction increased. [85]
One study explored the risk that one or more wisdom teeth will extracted in the future after having been decided to be retained. This study included a systematic literature review and included studies with greater than or equal to 50 patients and at least one asymptomatic wisdom tooth. They found the mean incidence rate for the extraction of previously asymptomatic retained wisdom teeth ranged from 5% at 1 year to 64% at 18 years, with extraction occuring mostly due to caries, periodontal disease and other inflammatory conditions. [86]
If a wisdom tooth has associated pathology such as that discussed below it is recommended to have that impacted wisdom tooth removed. Refer back to the wisdom teeth page for reasons and indications for having a wisdom tooth removed.
1. Gum Disease (Periodontal Disease / Periodontitis)
Wisdom teeth may break partway through the gums, causing a flap of gum tissue to grow over them. Food can become trapped under the flap and cause the gums to become red, swollen, and painful. These are signs that bacteria growing under the flap are causing infection. Gum disease (periodontal disease) may be initially mild known as gingivitis or progress to periodontitis.
Periodontal disease can harm the gums, potentially causing inflammation and bleeding. The gum can recess which can lead to bone loss around teeth. Tooth loss can occur. Even the neighboring tooth (known as the second molar) can be affected with potential infection and decay which could affect chewing. [22] The early stages of periodontitis can be difficult to detect as there can be no symptoms and no pain present even with chronic gingivitis present while the gums can also appear mostly normal. [66] Because of this, oral surgeons often recommend removal of the infected wisdom tooth or wisdom teeth to prevent damage or loss of an adjacent second molar.
In addition to destroying gum, bone, and even other teeth around an affected wisdom tooth, periodontal disease may have a negative impact on your general health. The American Association of Oral and Maxillofacial Surgeons (AAOMS) likes to use the phrase "the absence of clinical symptoms (asymptomatic) does not indicate absence of disease or pathology." Elevated levels of "red'' (B. forsythus, P. gingivalis and T. denticola) and ''orange'' (P. intermedia and C. rectus) complex microorganisms and increased levels of gingival crevicular fluid (GCF) inflammatory mediators interleukin 1-b (IL-1b) and prostaglandin E2 (PGE2) were found in people who had periodontal pockets which had probing depths of >= 5 mm. [17, 18, 21] These red and orange micoorganisms, in addition to others, have been shown to work in clusters as the causative agents for the initiation and propagation of periodontitis. [78]
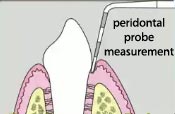
Periodontal probing depth is a measure of the space (pocket) between gum and tooth with a dental probe. There are typically 6 probing pocket depths around the wisdom tooth and two probing pocket depths of the adjacent tooth (second molar). A larger probing depth is more likely to collect microorganisms and reproduce. A periodontal probing depth of 3 mm or less is generally considered healthy. (A periodontal probing depth of greater than or equal 4 mm or when the attachment of the gum to the tooth (attachment loss) is 3 mm or more is used by AAOMS as a cutoff for when they feel wisdom teeth should be extracted due to the increased risk of developing periodontal disease. See the controversy page). [4, 21, 38, 45, 49]
An association between periodontal disease and systemic disease has been shown. It is possible that chronic periodontal infections results in inflammation which can lead to bacteria entering the bloodstream and may have a negative impact on general health and potentially lead to a harmful systemic impact. This could be due to an an immune system reaction and explain why increased inflammatory mediators were found. These potential systemic diseases that may be associated with periodontal disease include premature delivery of low-birth weight infants, coronary aftery disease, coronary heart disease, renal vascular disease, stroke, diabetes, bacterial pneumonia, chronic obstructive lung disease, and Alzheimer's disease. Hence, if pocketing around wisdom teeth is left untreated it can slowly spread and infect other sites in the mouth. [4, 13, 15, 16, 17, 18, 21, 22, 38, 54, 69, 70, 71]
A meta-analysis of 10 randomized trials in January 2011 found no evidence in favor of peridontal disease being associated with preterm births and low birth weight. [64] For those women trying to conceive it may take longer to get pregnant if you have gum disease. [72]
Many of these periodontal pockets can be cured with antibiotics, oral rinsing, or removal of excess tissue (the hyperculum) around the tooth, without requiring removal of the tooth itself. [14]
In regards to peridontal pathology, The Journal of Oral and Maxillofacial Surgeons (on behalf of AAOMS) has produced at least 7 papers examing 329 patients who had at least 1 asymptomatic wisdom tooth visible. [26, 28, 37, 39, 40, 41, 43] These small sample sizes composed mostly of the Caucasian population are not representative of the general population and as of such these findings cannot be applied to all clinical situations. A 2010 paper by authors from the University of Toronto's dental school provided some further discussion on these papers and results stating "most studies summarized their results as a percent difference between control groups but this difference cannot be compared for consistency between research papers." They further discussed how the studies did not make adjustments for potentially confounding factors such as smoking, diabetes, genetic predisposition, and type of bacterial populations which are all risk factors for peridontal disease. In addition these authors stated "loss to follow up creates further bias in these results; as the small sample sizes further decrease, the results may both overestimate and misrepresent the actual existing clinical situation, lessening the strength of evidence." [38] The key findings from these 7 papers are subsequently discussed in the following 5 paragraphs.
In a 329 patient study (median age 25) periodontal pockets which had depths of greater than or equal 5 mm with attachment loss in the wisdom tooth region occured in 82 of these patients (24.9%) with asymptomatic wisdom teeth which could potentially lead to periodontal disease. [26] If one of the 329 patients had at least 1 periodonal probing depth in the wisdom tooth region of greater than or equal to 4 mm than, after a period of about 2 years, 58 of these patients (38.4%) (of which 254 of the original 329 had follow up visits and 151 had at least 1 periodonal probing depth in the wisdom tooth region of greater than or equal to 4 mm at baseline) had their periodontal probing depth increase by 2 mm or more. In addition in this study periodonal probing depths in the wisdom tooth region of less than 4 mm than led to periodontal probing depth increase by 2 mm or more in 3 of these patients (2.91%). [28]
Asymptomatic erupted wisdom teeth with periodonal probing depths greater than or equal to 4 mm have an increased risk of developing further disease when compared to other healthy wisdom teeth. Using the same 329 patient study stated above, 195 patients of the patients over about 6 years (median age at enrollment 26.3) were examined. 122 had had at least 1 periodonal probing depth in the wisdom tooth region of greater than or equal to 4 mm at baseline and after the roughly 6 year study period amongst these 122 subjects there was an approximate 10% increase in also developing a periodonal probing depth greater than or equal to 4 mm in at least one non-wisdom tooth region. [37] In those 122 patients with at least 1 periodonal probing depth in the wisdom tooth region of greater than or equal to 4 mm at baseline there was an approximate 12 times likelyhood of periodontal pathology in the wisdom tooth after the roughly 6 year follow up. Further in these 122 patients there was an approximate almost 5 times likelyhood of disease in a non–wisdom tooth region after the roughly 6 year follow up. [39]
Using a subset of the same 329 patient study stated above, 106 of these patients were periodontally healthy in the wisdom tooth region at baseline and after a median of 4.1 years, 40 (37.7%) had at least 1 periodonal probing depth in the wisdom tooth region of greater than or equal to 4 mm. 20 of these 40 patients (50%) also had at least 1 periodonal probing depth in a non-wisdom tooth region of greater than or equal to 4 mm whereas 10 of the 66 patients (15.2%) who did not have at least 1 periodonal probing depth in a wisdom tooth region of greater than or equal to 4 mm also had at least 1 periodonal probing depth in a non-wisdom tooth region of greater than or equal to 4 mm. [40]
Again using this same 329 patient study who had at least 1 asymptomatic wisdom tooth visible, 329 patients where 2.5 times more likely to have periodontal pathology (at least 1 periodonal probing depth in a non-wisdom tooth region of greater than or equal to 4 mm) in the first and second molars when compared to the 69 patients also in the study (411 total patients) who had no visible wisdom teeth. [41]
Further using this same 329 patient study, 69 patients had wisdom teeth removed of which the reasons were not given. Around 26% of these patients saw improvement in their periodontal pathology (as in all periodonal probing depths less than 4 mm) at a median follow up time of 9 months after surgery when compared to enrollment in the study. [43]
Wisdom teeth with pre-exisiting periodontal pocketing or which have attachment loss that are extracted will most of the time either have their peridontal health improve or remain unchanged. [16, 31, 32]
In another study involving a subsample of 6,793 patients (ages 52 to 74) of participants from the Dental Atherosclerosis Risk in Communities (DARIC) study, 2,003 patients had at least 1 visible wisdom tooth. In these 2,003 patients having at least 1 periodonal probing depth in a non-wisdom tooth region was statistically significantly greater when compared to the patients who did not have a visible wisdom tooth. [42]
In a study looking at 5,831 individuals (ages 18 to 34) from the National Health and Nutrition Examination Survey (NHANES) III those with a visible wisdom tooth were 2.1 times more likely to have at least 1 periodonal probing depth greater than or equal to 5 mm in an adjacent second molar and 1.3 times more likely to have gingival bleeding in an adjacent second molar (tooth next to wisdom tooth). [44]
In a study looking at 9,182 adults ages 20 and older and meeting certain study inclusion criteria from the 1999 to 2004 National Health and Nutrition Examination Survey (NHANES), 1,024 (8.2%) of these individuals had periodontal disease. n-3 fatty acid intake (omega 3 fatty acids) particularly docosahexaenoic acid (DHA) intake and eicosapentaenoic acid (EPA), was found to be inversely associated with periodontitis. [50] Regularly taking a dietary supplement such as fish oil and/or regularly eating foods containing omega 3 fatty acids such as nuts, peanut butter, and salmon may thus be beneficial in helping to prevent periodontal disease. In addition ensuring you have enough vitamin D may also help prevent periodontal disease. [76]
Periodontal disease has been reported of occuring in 6% to 10% of all impacted wisdom teeth. [15]
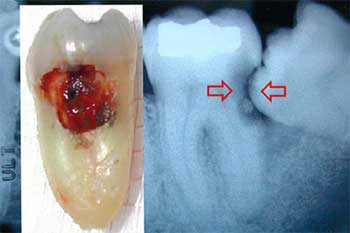
2. Cavity in a Tooth Next to a Wisdom Tooth
A wisdom tooth that is aligned poorly creates a trap for plaque and debris between the wisdom tooth and the adjacent second molar. This leads to cavities (decay - caries) which can occur.
Both a third molar and second molar can decay and develop a cavity and both may need to be extracted if the cavities become severe. The image to your right shows an example of this scenario.
Signs of decay which dental professionals check for include chalky enamel, stain, and soft tooth structure. [46]
One study has demonstrated that patients who have mandibular third molars with an angulation between 31 and 108 degrees, a distance of 3–10 mm to the second molar and those classified as horizontal or mesioangular, were most likely to be linked to distal caries on the adjacent second molar. [77]

3. Root, Bone, Crown Breakdown Next to/or To a Wisdom Tooth (Internal/External Resorption)
A dental crown, filling, and bridge (restorations) in a tooth next to/(or to) an impacted wisdom tooth could breakdown and become destroyed. Similary a root in a tooth next to/(or to) an impacted wisdom tooth could breakdown which could lead to loss of the root structure. In addition, bone could breakdown near a wisdom tooth. This would cause treatment to become necessary and could potentially lead to extraction being needed. This is also known as resorption.
Internal resorption has been reported of occuring in 0.85% of all impacted wisdom teeth, while resorption on a tooth next to a wisdom tooth has been reported of occuring in 4.78% of cases where an impacted wisdom tooth is present. [15]
4. Cavity in a Wisdom Tooth
If a wisdom tooth is hard to clean due to positioning, dental plaque can remain after and form a cavity. This is also known as food stagnation and food impaction.
A cavity in a wisdom tooth can be repaired by placing a filling as is normally done with other teeth. Some dentists will not fill a cavity in a wisdom tooth period or only in certain circumstances. This is because the decay found on the tooth might be in an awkward location making it challenging for a dentist to perform a restoration.
If a wisdom tooth with a cavity is filled, another cavity can form adjacent to an existing filling, especially if the tooth is hard to clean. If a cavity in a wisdom tooth is unrestorabled it will need to be extracted.
It has been shown that having cavities in teeth other than a wisdom tooth is a good indicator of whether or not a wisdom tooth may develop a cavity. In one study of 303 patients (median age 25.3) 1.32% had a cavity in a wisdom tooth without also having experiences of a cavity in a non-wisdom tooth. In this study 84 of those patients (27.72%) had at least one cavity experience in a wisdom tooth. [19] In another study involving a subsample of participants from the Piedmont 65+ study, 818 patients all over 65 years old, 8% had a cavity in a wisdom tooth without also having experiences of a cavity in a non-wisdom tooth. In this study 342 had a visible wisdom tooth while 96 of those patients (28%) had evidence of a cavity experience in a wisdom tooth. [27] In yet another study involving a subsample of participants from the Dental Atherosclerosis Risk in Communities (DARIC) study, 6,650 patients with ages between 52 and 74, 1% of those had a cavity in a wisdom tooth or existing restoration (indicating a previous cavity in that wisdom tooth) without also having evidence of a cavity or restoration in a non-wisdom tooth. In this study, 2,003 patients had a visible wisdom tooth with 1,550 of those patients (77%) having evidence of a cavity or restoration (indicating previous cavity) in a wisdom tooth. [20] Further analysis of the DARIC study, using 1,993 patients who had a visible wisdom tooth and data available for both caries experience and periondontal pathology showed 68% had both cavity experience and periodontal pathology and less than 2% had no experiences of a cavity and no periodontal pathology. [48]
In one study, 409 patients with an average age of 25 years old were explored. 24% of these patients had wisdom teeth caries experience. Further, only 3 subjects (<1%) had caries experience exclusively on a wisdom tooth. 229 patients had all third molars at the occlusal plane. One quarter of this subset of patients (26%) were affected by both wisdom tooth caries experience and at least 1 periodontal probing site of 4 mm or more. Only 16% of patients had no cavities in a wisdom tooth and no periodontal problems. [83]
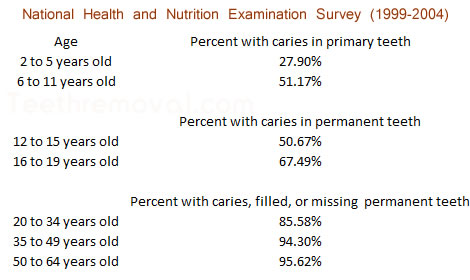
Data from the 1999 to 2004 National Health and Nutrition Examination Survey (NHANES) by the Centers for Disease Control and Prevention / National Center for Health Statistics supported by the United States Federal Government has shown the following ages and percentages of those who have had at least one dental carie (cavity), at least one tooth missing, and/or at least one permanent tooth filled. [25]
An x-ray is needed to help detect the presence of a cavity. What a person eats and drinks (their diet) can contribute to cavity formation. Regularly drinking acidic drinks such as soda (pop) can accelerate tooth decay and so can eating sticky candy, dried fruit, and sweet foods.
5. Pericoronitis (Infection of Gum Tissue)
When a wisdom tooth does not come out fully through the gums and into its proper position (meaning partially erupted) this can create an extension of gum called an operculum. This operculum can be irritated and infected leading to pericoronitis which means that bacteria and debris have collected under the overlying flap of gum tissue and their is an active infection and inflammation.
The signs of pericoronitis are tenderness, pain, bad taste, swelling in the gum tissue surrounding a wisdom tooth, swelling of the face, and difficulty opening the mouth (trismus).
There can also be an unpleasant mouth odor, severe pain, and a bad taste coming from the infected area. Usually a dentist will show patients how to flush out and irrigate the space between the tooth and gum where the infection is. Antibitoics are often given.
If the wisdom tooth is impacted, pericoronitis will often come back after it has cleared up which is known as recurrent periocoronitis. Under the right conditions when an operculum is present and if the wisdom tooth has already erupted, it is possible to make an operculectomy, which is the removal of the extension of the gum without extracting the tooth. Hence, it is important for a dentist to determine if a partially erupted wisdom tooth causing pericoronitis will continue to erupt normally or if it will remain impacted. Having an impacted wisdom tooth (partially erupted) with recurrent periocoronitis will likely need to be extracted.
One person from the U.K. sent an email in August 2011 saying the following:
In May 2009, I noticed that my upper left Wisdom Tooth was breaking through (age 46). My dentist assured that all was well and nothing to worry about. A year later I suffered a severe pain all along my left gums. I was told "Oh the wisdom tooth has pulled through the gums". My dentist did not elaborate that this was a common gum infection caused by partial wisdom teeth eruption called pericoronitis...I was given antibiotics which cleared the pain but left a slight tenderness in the gums (I did not realise that the infection was still there). Three months later I developed a gum abscess on the 1st molar which was treated with antibiotics and kept pussing for days on end. A month later the 1st molar broke in half and had to be extacted. The dentist still did not recommend extraction of the wisdom tooth. A month later I noticed that my bite was changing as the wisdom tooth was pushing the 2nd Molar. By now I was in absolute panic as I knew that I was going to loose the 2nd molar so the dentist agreed to book me in for a private extaction with a specialist. The Specialist extracted the wisdom for £100 and recommended a dental implant to replace the missing tooth for £4000. In my view all partial eruptions must be extracted immediately in order to avoid further complications and expense.
In some cases pericoronitis can lead to significant life threatening infections and antibiotics followed by surgical removal of the tooth associated with the infection may be promptly needed. [4]
Pericoronitis has an average of 8% incidence associated with wisdom teeth. However, this number includes single episodes of pericoronitis and a wisdom tooth with pericoronitis typically is only extracted if recurrent periocoronitis as in additional episodes occur. [15]
6. Cysts/Tumor Development
A fluid sac may form around an impacted tooth, and the sac may grow into a cyst, which can cause permanent damage to healthy teeth, jawbone, nerves, and bones and possibly lead to fracture. Rarely a tumor may develop, which can require removal of tissue and bone. Cysts and/or tumors require an x-ray in order to detect their presence.
Studies indicate that cysts and tumors develop somewhere in the range of 1% to 3% of all impacted wisdom teeth. [10, 52, 69, 75]
7. Additional Considerations
One or more wisdom teeth may come in at an awkward angle, with the top of the tooth facing forward, backward, or to either side. Unpredictable changes in the position and angulation of wisdom teeth can occur after the teenage years. [33, 35] This can potentially lead to a cavity in a tooth next to a wisdom tooth (adjacent 2nd molar) and also can potentially cause the gums to recede around the tooth. [24]
A wisdom tooth may even remain trapped beneath the gum and bone. There may not be enough room in the jaw for the wisdom tooth to erupt and come through. Some wisdom teeth may not be able to fully erupt and hence remain partially erupted which could potentially result in gum pain. [24]
Some wisdom teeth can not be properly cleaned such as if the external oblique ridge of the mandible prevents cleaning of lower wisdom teeth or the cornoid process of the mandible prevents cleaning of the upper wisdom teeth. This can lead to an increased risk of developing problems such as those stated above and below. [23, 24]
A wisdom tooth could cause pain unrelated to other conditions and not due to normal pain experience when it first grows in or even after growing in.
If orthodontic treatment such as braces is needed, keeping wisdom teeth may affect the treatment. Even so many wisdom teeth extracted for orthodontic treatment may be prematurely or unecessarily extracted and proper consideration of the planned orthodontic extraction treatment plan and facial growth related changes should be taken into account. [16]
If a patients jaw is not not wide enough their wisdom teeth may erupt in an alignment that can cause problems with the way they chew food. This could lead to pain in the jaw joint as in Temporomandibular Joint Syndrome (TMJ).
A cavity in a tooth next to a wisdom tooth or periodontal pockets present in a tooth next to a wisdom tooth, may benefit from extraction. [13]
If one has a specific medical and/or surgical condition removing wisdom teeth may in some cases be warranted.
If one has a certain lifestyle or job that may in the future prevent them from being able to receive dental treatment in a timely matter removing wisdom teeth may in some cases be warranted.
A wisdom tooth can become infected which may require it to be extracted or treated with root canal so that no active infection is present. Gum disease, tooth decay, and necrosis of the tooth's nerve can lead to an abscess. Further problems that can occur include cellulitis, osteomyeletis, mandibular fracture, tooth fracture, and Temporomandibular Joint Syndrome (TMJ) symptoms, and chronic headache. An infected wisdom tooth could also lead to single-space and multi-space infections around your head and neck. One may notice symptoms such as drainage of pus, swelling, significant fever, pain, difficulty swallowing, difficulty breathing, and difficulty opening the mouth. This can lead to/ be diagnosed as such things as sepsis, Ludwig's angina, descending necrotizing mediastinitis, cavernous sinus thrombosis, necrotizing fasciitis, mucormycosis, and death. This can be the result of a wisdom tooth that is difficult to clean. A large amount of face, throat, and neck swelling can cause difficulty breathing and may require an emergency tracheotomy to open and preserve the airway. Subsequent surgery or surgeries may be required for drainage. This may require immediate medical treatment with IV antibiotic therapy and an extended hospital stay. The risks described in this final paragraph also can happen as a complication of removing an impacted wisdom tooth. More details are discussed on the wisdom teeth removal complications section. More severe complications of surgery may occur in wisdom teeth removed that are diseased (with pathology) than in wisdom teeth removed that are healthy. Ice and heat should not be used for treatment when a wisdom tooth is infected. [12, 58, 59, 60, 62, 63, 65]
As mentioned above, a wisdom tooth with an abscess can be dangerous since the root structure extends a considerable distance down the throat and neck and can readily lead to rapid, systemic progression of infection to other parts of the body and develop into sepsis. In California, a man with an abscessed wisdom tooth developed sepsis which spread systemically leading to his death. He had had chronic gum disease and infection present for 2 years prior and was referred for extraction but never had the surgery performed. [61]
If you do not have health insurance and have very little money keeping wisdom teeth can potentially be dangerous as this may prevent you from getting dental care if the need arises. A 24 year old man in Ohio experienced pain in one of his wisdom teeth and was told to have it extracted. He did not have/ pay for the extraction and did not have/ pay for antibiotics. The infection eventually spread to his brain and he died. [73, 74]
A 23 year old obese man in Nevada had difficulty swallowing and pain and swelling in his jaw. He went to a hospital and was found to have a severe wisdom tooth infection with submandibular/ sublingual cellulitis which soon progressed to Ludwig's angina. This lead to surgery to remove his lower wisdom teeth by an oral surgeon. During the surgery the anesthesiologist incorrectly used an LMA airway device instead of an Endotracheal tube to keep his airway open to allow him to breathe. His airway was not open for 11 minutes and this lead to a severe brain injury and later brain death. [68]
Updated Dec. 4, 2016
References
1. MayoClinic. Impacted Wisdom Teeth. Accessed July, 2008. https://www.mayoclinic.org/diseases-conditions/wisdom-teeth/symptoms-causes/syc-20373808
2. Friedman JW. The prophylactic extraction of third molars: a public health hazard. Am J. Public Health 2007;97:1554-1559.
3. Jeannette Curtis, Healthwise. Written September, 2007.
http://www.webmd.com/oral-health/wisdom-tooth-extraction
4. American Association of Oral and Maxillofacial Surgeons. White Paper on Third Molar Data.
Written March 2007.
5. WMDS, Inc. Impacted Wisdom Teeth. Accessed July 31, 2008.
http://www.animated-teeth.com/wisdom_teeth/t2_wisdom_tooth_extraction.htm
6. Flickr.com. Image by samfeinstein. http://www.flickr.com/photos/samfeinstein/1349509551/
7. Dr. Anto Youssef, Studio Dentaire http://www.studiodentaire.com/en/treatments/wisdom_teeth.php#expression
8. Brauer HU. Quintessence International. Unusual Complications Associated with Third Molar Surgery: A Systematic Review. 2009. July-Aug. vol. 40. issue 7. pages 565-562.
9. Removal of Third Molars. National Institutes of Health Consensus Statement. Nov. 28-30, 1979. vol. 2. issue 11. pages 65-68. http://consensus.nih.gov/1979/1979Molars021html.htm
10. Panagiotis Stathopoulos and et. al. Cysts and Tumors Associated with Impacted Third Molars: Is Prophylactic Removal Justified? J Oral Maxillofac Surg. Vol. 69. Issue 2. pages 405 - 407. 2011.
11. Current Clinical Practice and Parameters of Care: The Management of Patients with Third Molar Teeth. Faculty of Dental Surgery. The Royal College of Surgeons of England. London.
September 1997.
12. Tung-Yiu Wong. A Nationwide Survey of Deaths From Oral and Maxillofacial Infections: The Taiwanese Experience. J Oral Maxillofac Surg. 57. pages 1297-1299. 1999.
13. Thomas B. Dodson and Srinivas M. Susarla. Impacted Wisdom Teeth. Search date July 2009. Clinical Evidence. 2010. 04:1302. pages 1- 17.
14. J. W. Friedman FRIEDMAN RESPONDS Am J Public Health, April 1, 2008; 98(4): 582 - 582.
15. Friedman JW. The prophylactic extraction of third molars: a public health hazard. Am J. Public Health 2007;97:1554-1559. http://www.ajph.org/cgi/content/full/97/9/1554
16. S Kandasamy and DJ Rinchuse.
The wisdom behind third molar extractions. Australian Dental Journal. 54. pages 284-292. 2009. http://onlinelibrary.wiley.com/doi/10.1111/j.1834-7819.2009.01152.x/abstract
17.
Raymond P. White and et. al. Microbial Complexes Detected in the Second/Third Molar Region in Patients With Asymptomatic Third Molars. J Oral Maxillofac Surg. vol. 60. pages 1234-1240. 2002.
18. Raymond P. White and et. al. Inflammatory mediators and periodontitis in patients with asymptomatic third molars. J Oral Maxillofac Surg. vol. 60 pages 1241–1245. 2002.
19. Daniel A. Shugars and et. al.
Occlusal Caries Experience in Patients with Asymptomatic Third Molars. J Oral Maxillofac Surg. vol. 62. pages 973-979. 2004.
20. Elda L. Fisher and et. al. Third Molar Caries Experience in Middle-Aged and Older Americans: A Prevalence Study.
J Oral Maxillofac Surg. vol. 68. pages 634-640. 2010.
21. American Association of Oral and Maxillofacial Surgeons. Third Molar Multidiscplinary Conference. October 19, 2010.
22. Linda Humphrey and et al. Periodontal Disease and Coronary Heart Disease Incidence:
A Systematic Review and Meta-analysis. J Gen Intern Med. vol. 23. issue 12. pages 2079-2086. 2008.
23. Scott Frey. Dentist. Responses to Should I get my wisdom teeth out if they are not bothering me? Asked by Mary Cheever.
http://www.quora.com/Should-I-get-my-wisdom-teeth-out-if-they-are-not-bothering-me Accessed February 10, 2011.
24. Tom. Dental Student. Why Dentists Extraction Wisdom Teeth. August 16, 2010. http://www.oralanswers.com/2010/08/why-do-wisdom-teeth-have-to-get-pulled/ Accessed February 10, 2011.
25. National Institute of Dental and Craniofacial Research. National Institutes of Health.
http://www.nidcr.nih.gov/DataStatistics/FindDataByTopic/DentalCaries/ National Health and Nutrition Examination Survey. 1999-2004.
26. George H. Blakey and et al. Periodontal Pathology Associated with Asymptomatic Third Molars.
J Oral Maxillofac Surg. vol. 60. pages 1227-1233. 2002.
27. Kevin. L. Moss and et al. Third Molar Periodontal Pathology and Caries in Senior Adults.
J Oral Maxillofac Surg. vol. 65. pages 1-3-108. 2007.
28. George H. Blakey and et al. Progression of Periondontal Disease in the Second/Third Molar Region in Subjects With Asymptomatic Third Molars.
J Oral Maxillofac Surg. vol. 64. pages 189-193. 2006.
29. C.M. Hill and R. V. Walker. Conservative, non-surgical management of patients presenting with impacted third molars: A 5 year study.
Br J Oral Maxillofac Surg vol. 44. pages 47–50. 2006.
30. Irja Venta and et al. Long-Term Evaluation of Estimates of Need for Third Molar Removal.
J Oral Maxillofac Surg. vol. 58. pages 288-291. 2000.
31. Thomas B. Dodson. Response to APHA C3: Oppostion to Prophylactic Removal of Third Molars. October 26, 2008.
32. Daniel T. Richardson and Thomas B. Dodson. Risk of periodontal defects after third molar surgery: An exercise in evidence-based clinical decision making. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. vol. 100. no. 2. August 2005.
33. Sumeet Sandhu and Tejinder Kaur. Radiographic Study of the Positional Changes and Eruption of Impacted Third Molars in Young Adults of the Asian Indian Population.
J Oral Maxillofac Surg. vol. 66. pages 1617-1624. 2008.
34.
Esther Kruger and et al. Third molar outcomes from age 18 to 26: Findings from a population-based New Zealand longitudinal study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. vol. 92. pages 150-155. 2001
35. Faiez N. Hattab. Positional changes and eruption of impacted mandibular third molars in young adults: A radiographic 4 year follow-up study.
Oral Surg Oral Med Oral Pathol Oral Radiol Endod. vol. 84. pages 604-608. 1997.
36. Irja Venta and et al. Clinical Outcome of Third Molars in Adults Followed During 18 Years.
J Oral Maxillofac Surg. vol. 62. pages 182-185. 2004.
37. George H. Blakey and et al. Changes in Third Molar and Nonthird Molar Periodontal Pathology Over Time.
J Oral Maxillofac Surg. vol. 65. pages 1577-1583. 2007.
38. Bertha Luk and et al. Prophylactic Extraction of Asymptomatic Third Molars to Prevent Periondontal Pathology: An Evidence Based Study.
Community Dentistry DEN207Y. University of Toronto. April 8, 2010.
39. Raymond P. White and et al. Risk markers for periodontal pathology over time in the third molar and non‐third molar regions in young adults. J Oral Maxillofac Surg. vol. 66. pages 749‐754. 2008.
40. George H. Blakey and et al. Changes over time in the periodontal status of young adults with no third molar periodontal pathology at enrollment. J Oral Maxillofac Surg. vol. 67. pages 2425‐2430. 2009.
41. George H. Blakey and et al. Third molars and periodontal pathology in American adolescents
and young adults: a prevalence study. J Oral Maxillofac Surg. vol. 68. pages 325‐329. 2010.
42. Kevin L. Moss and et al. Third molars and periodontal pathologic findings in middle‐age and older Americans. J Oral Maxillofac Surg. vol. 67. pages 2592‐2598. 2009.
43. George H. Blakey. Impact of removal of asymptomatic third molars on periodontal pathology. J Oral Maxillofac Surg. vol. 67. pages 245‐250. 2009.
44. John R. Elter and et al. Third molars associated with periodontal pathology in the Third National Health and Nutrition Examination Survey. J Oral Maxillofac Surg. vol. 62. pages 440‐445. 2004.
45. David Leader. How Gum Disease Affects your Health.Will Periodontitis Make You Sick? December 23, 2010. associatedcontent.com
46. David Leader. The Dental Examination. Just a Check Up. January 15, 2009. associatedcontent.com
47. Faiez N. Hattab. Positional Changes and Eruption of Impacted Mandibular Third Molars in Young Adults. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. vol. 84. pages 605-608. 1997.
48. Rachel Garaas. Prevalence of Visible Third Molars With
Caries Experience or Periodontal Pathology in Middle-Aged and Older Americans. J Oral Maxillofac Surg. vol. 69. pages 463-470. 2011.
49. Raymond P. White and et al. Visible Third Molars as Risk Indicator for Increased Periodontal Probing Depth.
J Oral Maxillofac Surg. vol. 69. pages 92-103. 2011.
50. Asghar Z. Naqvi and et al. n-3 Fatty Acids and Periodontitis in US Adults. Journal of the American Dietetic Association. vol. 110. issue 11. pages 1669-1675. 2010.
51. Fernandes MJ and et al. Actuarial life-table analysis of lower impacted wisdom teeth in general dental practice. Community Dent Oral Epidemiol. vol. 38. pages 58–67. 2010.
52. Wasiu Lanre Adeyemo. Do pathologies associated with impacted lower third molars justify
prophylactic removal? A critical review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. vol. 102. pages 448-452. 2006.
53. Paige E. Nance and et al. Change in Third Molar Angulation and
Position in Young Adults and Follow-Up Periodontal Pathology. J Oral Maxillofac Surg. vol. 64. issue 3. pages 424-428. 2006.
54. American Dental Association. Toothflix DVD series. Preventing Periodontal Disease.
55. National Institute for Health and Clinical Excellence. NICE issues guidance on frequency of dental check-ups. October 27, 2004.
56. National Institute for Health and Clinical Excellence. Dental recall: Recall interval between routine dental examinations.
Clinical Guideline 19. October 2004.
57. Department of Health. NICE recall intervals and oral health. A briefing for dentists and practice teams. Annex: NICE Recall Intervals and Oral Health. Gateway Approval Reference Number: 15654. March 2011. http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/documents/digitalasset/dh_126005.pdf
58. Susanne Kinzer and et al. Severe deep neck space infections and mediastinitis of odontogenic origin: clinical relevance and implications for diagnosis and treatment. Acta Oto-Laryngologica. 129. pages 62-70.
2009.
59. Jim deMaine MD. A Fatal Tooth Extraction. February 28, 2011. http://www.endoflifeblog.com/2011/02/fatal-tooth-extraction.html Accessed May 21, 2011.
60. Martin Kunkel and et al. Severe Third Molar Complications Including Death—Lessons from 100 Cases Requiring Hospitalization. J Oral Maxillofac Surg. 65. pages 1700-1706. 2007.
61. Dorothy Buckley v. John D. Durney.
C060340. Court of Appeals of California, Third Appellate District. June 7, 2010.
62. Sung-Kiang Chuang, David H. Perrott, and Thomas B. Dodson. Age as a Risk Factor for Third Molar Surgery Complications. J Oral Maxillofac Surg. vol. 65. issue 9. pages 1685-1692. 2007.
63. Griffin v. Bankston et al.
A08A2332. Court of Appeals of Georgia, First Division. December 24, 2008.
64. Mariana Fampa Fogacci and et al. The Effect of Periodontal Therapy on Preterm Low Birth Weight: A Meta-Analysis. Obstetrics & Gynecology. vol. 117. issue 1. pages 153-165. January 2011.
65. H. Ryan Kazemi DMD. Infection. 2011.
66. Jay W. Friedman DDS, MPH. The Intelligent Consumer's Complete Guide to Dental Health: How to Maintain Your Dental Health and Avoid Being Overcharged and Overtreated. 2002.
67. United States Department of Agriculture. http://www.choosemyplate.gov/ Accessed July 15, 2011.
68. Board of Medical Examiners of the State of Nevada. Complaint Against Steve Wong. Case No. 10-12651-1. June 29, 2011.
69. Sanjivan Kandasamy. Evaluation and management of asymptomatic third molars: Watchful monitoring is a low-risk alternative to extraction. American Journal of Orthodontics and Dentofacial Orthopedics. Vol. 140. Issue 1.
pages 11-17. July 2011.
70. S Paju and FA Scannapieco. Oral biofilms, periodontitis, and pulmonary infections. Oral Dis. 13. pages 508-512. 2007.
71. Angela R. Kramer and et al. Inflammation and Alzheimer's disease: Possible role of periodontal diseases.
Alzheimer's & Dementia. 4. pages 242–250. 2008.
72. European Society of Human Reproduction and Embryology. Gum disease can increase the time it takes to become pregnant. July 5, 2011.
73. Lukas I. Alpert. Daily News. Unemployed man with no health insurance dies after minor tooth infection spreads to brain. September 5, 2011.
http://www.nydailynews.com/news/national/2011/09/05/2011-09-05_unemployed_man_with_no_health_insurance_dies_after_minor_tooth_infection_spreads.html?r=news Accessed September 7, 2011.
74. Cincinnati Enquirer. Lauren Bishop. Bootsy Collin's newphew dies after tooth infection. September 2, 2011.
75. P. Stathopoulos and et al. Cysts and tumors associated with impacted third molars: is prophylactic removal justified? J Oral Maxillofac Surg. vol. 69. issue 2. pages 405-408. February 2011.
76. Laura McMahon and et al. Vitamin D-Mediated Induction of Innate Immunity in Gingival Epithelial Cells. Infection and Immunity. Vol. 79, No. 6, pages 2250-2256, June 2011.
77. S. G. M. Falci and et. al. International Journal of Oral and Maxilofacial Surgery. pp. 1270-1274, October 2012.
78. AAOMS. Advocacy White Paper on Evidence Based Third Molary Surgery
79.Ceib Phillips and Raymond P. White, How Predictable Is the Position of Third Molars Over Time? J Oral Maxillofac Surg. vol. 70, issue 9, supplement 1, pages 11-14, 2012.
80. Ceib Phillips and et al. Changes over time in position and periodontal probing status of retained third molars. J Oral Maxillofac Surg. vol. 65, pages 2011-2017, 2007.
81. Thomas B. Dodson. How Many Patients Have Third Molars and How Many Have One or More Asymptomatic, Disease-Free Third Molars? J Oral Maxillofac Surg. vol. 70, issue 9, supplement 1, pages 4-7, 2012.
82. Robert D. Marciani. Is There Pathology Associated With Asymptomatic Third Molars? J Oral Maxillofac Surg. vol. 70, issue 9, supplement 1, pages 15-19, 2012.
83. Rachel N. Garaas and et al. Prevalence of third molars with caries or periodontal pathology in young adults.
J Oral Maxillofac Surg. vol. 70, pages 507-513, 2012.
84. V. Toedtling and J. M. Yates.Revolution vs status quo? Non-intervention strategy of asymptomatic third molars causes harm. British Dental Journal. vol. 219, no. 1, pp. 11-12. July 10, 2015.
85. McArdle, L, and Renton.: The effects of NICE guidelines on the management of third molar teeth, British Dental Journal. E8. Sept 7, 2012.
86. G. Bouloux, K. Busaidy, O. Biern, S. Chuang, and T. Dodson. What is the risk of future extraction of asymptomatic third molars? A systematic review. J Oral and Maxillofac Surg. vol. 7, no. 5, pp. 806-11, 2015.
|